
Necrotizing meningoencephalitis in dogs is a rare and devastating condition that affects the brain and meninges, the protective membranes surrounding the brain and spinal cord. It's a serious disease that requires immediate veterinary attention.
This condition is also known as Canine Necrotizing Meningoencephalitis, or CNM for short. It's a progressive and irreversible disease that can cause seizures, tremors, and loss of coordination in dogs.
Dogs of any age can be affected by CNM, but it's most commonly seen in middle-aged to older dogs. The exact cause of CNM is still unknown, but it's believed to be related to a viral or bacterial infection that triggers an inflammatory response in the brain.
Symptoms of CNM can vary depending on the severity of the disease, but they often include changes in behavior, difficulty walking, and seizures.
You might enjoy: Can Allergies Cause Swollen Lymph Nodes in Dogs
Causes and Symptoms
Necrotizing meningoencephalitis is a serious condition that affects the brain of dogs, causing a range of symptoms.
Symptoms can vary depending on the part of the brain affected, but common signs include seizures, blindness, circling, abnormal mentation, and behavior changes.
Dogs with forebrain involvement may experience seizures, blindness, and changes in mental status, while those with brainstem involvement may exhibit head tilt, falling, deafness, facial paralysis, and limb weakness.
Here is a list of possible symptoms:
- Seizures
- Blindness
- Circling
- Abnormal mentation
- Behavior changes
- Difficulty walking
- Cervical pain
- Fever
- Head tilt
- Falling
- Facial paralysis
- Difficulty swallowing
- Limb weakness
Inflammation in the meninges of the brain can cause cervical rigidity, pain, and fever, while lesions in the brainstem can lead to more severe symptoms, such as paralysis and difficulty swallowing.
What Are?
Necrotizing meningoencephalitis is an inflammatory disease of the central nervous system.
The disease was first recognized in the United States during the 1970's, initially in pugs and known as pug dog encephalitis.
It wasn't until 1989 that the disease was recognized in other small breeds of dogs, and it can occur in either sex.
Lesions in necrotizing meningoencephalitis are typically very inflammatory with meningitis.
The disease has a rapid onset and progression, leading to death in dogs within a few months.
The lesions are usually located in the cerebellum, brainstem, and spinal cord, with a minimal amount of inflammatory lesions present.
Clinical Features
If your dog is experiencing seizures, blindness, or abnormal behavior, it could be a sign of necrotizing meningoencephalitis. This condition affects the brain and can cause a range of symptoms.
The forebrain is the part of the brain most often affected, leading to seizures, blindness, and changes in mental status. Lesions in this area can cause significant problems.
Inflammation in the meninges, the protective membranes surrounding the brain, can cause cervical rigidity, pain, and fever. This is a serious symptom that requires immediate attention.
Symptoms of necrotizing meningoencephalitis can vary depending on the part of the brain affected. If the brainstem is impacted, your dog may experience head tilt, falling, deafness, facial paralysis, and weakness in the muscles used for swallowing.
If you notice any of these symptoms in your dog, it's essential to make an appointment with your veterinarian as soon as possible. They will conduct a complete physical examination and ask you questions about your dog's symptoms and medical history.
Here are some common symptoms of necrotizing meningoencephalitis:
- Seizures
- Blindness
- Circling
- Abnormal mentation
- Behavior changes
- Difficulty walking
- Back pain
- Fever
- Head tilt
- Falling
- Facial paralysis
- Difficulty swallowing
- Limb weakness
Diagnosis and Treatment
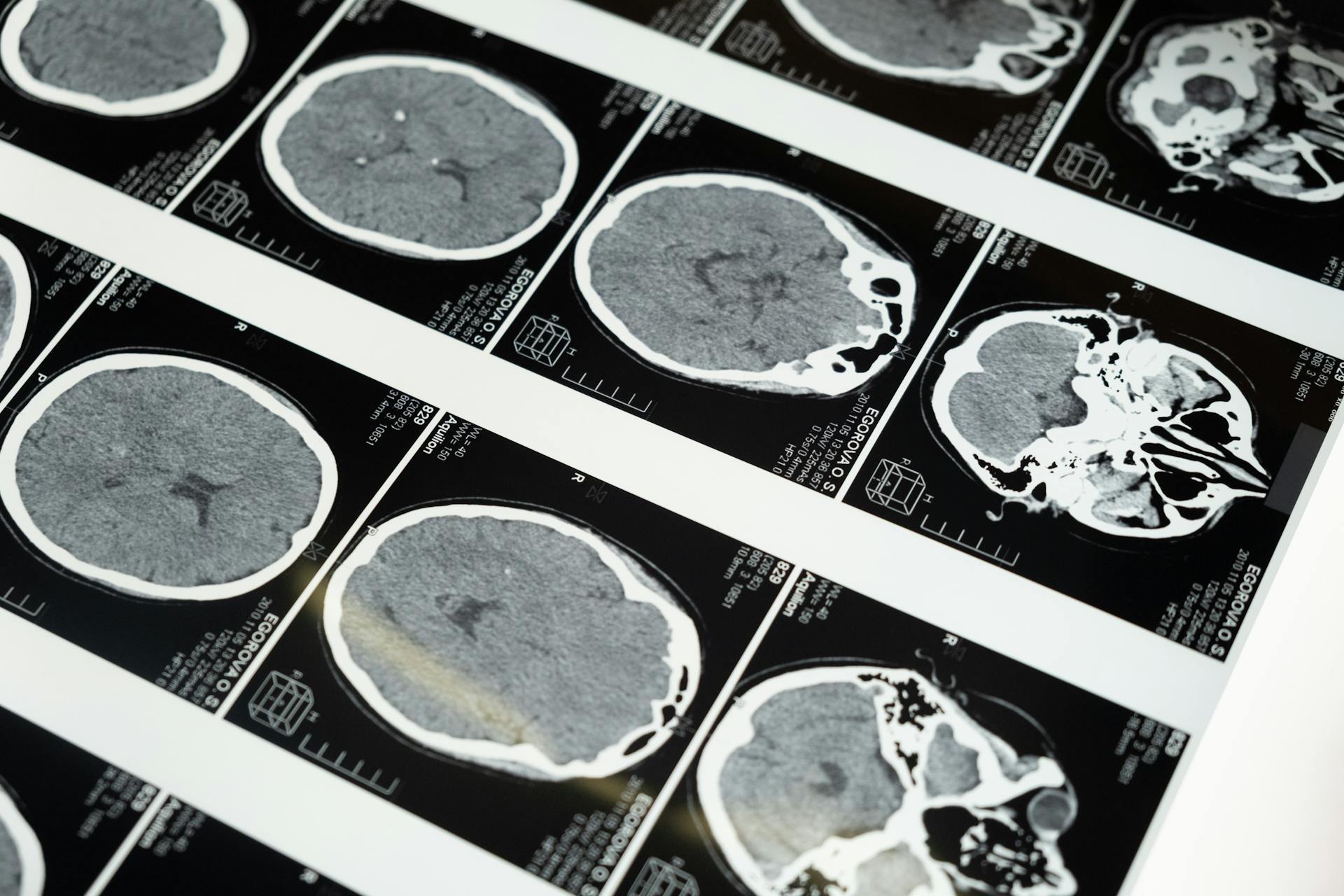
Diagnosis of necrotizing meningoencephalitis involves a series of tests, including an MRI, which is the most reliable way to diagnose the condition in a living animal.
Your veterinarian may recommend an MRI to get a clear picture of the brain and identify any lesions or cystic areas caused by the condition. Asymmetric, bilateral lesions in the forebrain and cystic areas in necrotic parts of the brain are typical findings on the imaging.
A cerebrospinal fluid (CSF) tap and/or an electroencephalogram (EEG) may also be recommended to rule out other causes of brain inflammation and confirm the diagnosis.
The goal of treatment is to provide supportive care and minimize symptoms, but the prognosis is poor even with aggressive treatment.
Treatment options include anticonvulsants, corticosteroids, anti-inflammatory medication, chemotherapy, rest, and ensuring proper nutrition and fluid intake.
Here are some treatment options your veterinarian may recommend:
- Anticonvulsants (for example phenobarbital) to treat seizures
- Corticosteroids (for example dexamethasone or prednisone) to suppress your dog’s immune system and prevent additional destruction
- Anti-inflammatory medication
- Chemotherapy
- Rest
- Ensuring nutrition and necessary fluid intake to help your dog fight the inflammation
Diagnosis in Dogs
Your veterinarian may recommend an MRI to diagnose necrotizing meningoencephalitis in your dog, as it's the most reliable way to make a diagnosis.
MRI findings typically include asymmetric, bilateral lesions in the forebrain, and cystic areas in the parts of the brain that are necrotic.
A cerebrospinal fluid (CSF) tap and/or an electroencephalogram (EEG) may also be recommended to help diagnose the condition.
A bacterial and viral culture of CSF and serological testing can help rule out other causes of brain inflammation and identify necrotizing meningoencephalitis.
Magnetic resonance imaging can also identify a mass effect in the cerebral hemisphere, causing compression of the lateral ventricle and displacement of the falx cerebri.
The imaging may show an ill-defined lesion with high signal intensity on T2-weighted images and fluid-attenuated inversion recovery images.
The lesion may also be iso- or hypointense to normal gray matter on T1-weighted images.
After IV administration of gadopentate dimeglumine, there may be mild, heterogeneous enhancement of brain parenchyma throughout the lesion as well as in the adjacent leptomeninges.
This can help your veterinarian make a more accurate diagnosis and develop an effective treatment plan for your dog.
See what others are reading: How to Help Dogs with Skin Allergies
Treatment of Dogs
Your veterinarian may recommend an MRI to diagnose necrotizing meningoencephalitis, which can show asymmetric, bilateral lesions in the forebrain and cystic areas in the necrotic parts of the brain.
A cerebrospinal fluid (CSF) tap and/or an electroencephalogram (EEG) may also be recommended to rule out other causes of brain inflammation.
Treatment goals are to provide supportive care and minimize symptoms, as the prognosis is poor even with aggressive treatment.
Typical treatment options include anticonvulsants to treat seizures, corticosteroids to suppress the immune system, anti-inflammatory medication, chemotherapy, rest, and ensuring nutrition and necessary fluid intake.
- Anticonvulsants (for example phenobarbital) to treat seizures
- Corticosteroids (for example dexamethasone or prednisone) to suppress the immune system and prevent additional destruction
- Anti-inflammatory medication
- Chemotherapy
- Rest
- Ensuring nutrition and necessary fluid intake to help your dog fight the inflammation
The prognosis for dogs with necrotizing meningoencephalitis is poor, and most dogs die or are euthanized within six months of their symptoms first becoming apparent.
Histopathological Features
Histopathological features play a crucial role in diagnosing and understanding the underlying causes of brain inflammation. The inflammation is characterized by a non-suppurative nature, with lymphoplasmacytic and histiocytic cells infiltrating the meninges and causing necrotizing changes in the corona radiata, thalamus, and cerebrocortical area.
The meninges are focally thickened due to the infiltration of lymphocytes, plasma cells, and macrophages, which is a result of the immune system's response to the inflammation. This leads to perivascular cuffing, a condition where blood vessels are surrounded by immune cells.
The encephalic lesions in the corona radiata are multifocal and can be divided into three phases: acute, subacute, and chronic. The acute phase is characterized by mild inflammatory cell infiltration, while the subacute phase shows intense inflammatory reactions. The chronic phase is marked by an increase in perivascular cuffing and extensive necrosis.
These lesions can be observed in the temporal lobes, where dense mononuclear cells infiltrate the meninges, and in the cerebellum, where herniation through the foramen magnum can occur. This can lead to neurological symptoms such as continuous circling or stroke-like seizures.
Here's a breakdown of the three phases of encephalic lesions:
- Acute: mild inflammatory cell infiltration
- Subacute: intense inflammatory reactions
- Chronic: increase of perivascular cuffing, extensive necrosis
Microscopically, blood vessels in the meninges, gray matter, and white matter are cuffed by a large number of lymphocytes and plasma cells, with fewer macrophage and occasional neutrophils. Neuronal necrosis and depletion, marked gliosis, and areas of mild cavitation with gitter cell accumulation are also present throughout the cerebrum.
Discussion
Diagnosis is a crucial step in determining the best course of treatment. A doctor will typically conduct a physical examination and take a thorough medical history to identify symptoms and potential causes.
The symptoms of a condition can vary widely, but often include pain, fatigue, and difficulty performing daily activities. This is why a doctor will ask detailed questions about a patient's symptoms and medical history.
A diagnosis can be made through various methods, including imaging tests, laboratory tests, and biopsies. These tests can help identify the underlying cause of symptoms and guide treatment decisions.
Treatment options will depend on the underlying cause of symptoms and the severity of the condition. In some cases, treatment may involve medication or lifestyle changes, while in other cases, more invasive procedures may be necessary.
A doctor will work closely with a patient to develop a personalized treatment plan that takes into account their unique needs and circumstances. This may involve regular check-ins and adjustments to the treatment plan as needed.
Research and Methods
To understand Necrotizing meningoencephalitis (NME), researchers reviewed archives from 3 institutions and 1 author's collection to identify confirmed cases.
They looked for histopathologically confirmed cases in breeds where the disease hadn't been reported before.
The researchers evaluated age, sex, breed, survival from the onset of clinical signs, and histopathologic findings.
Hypothesis/Objectives
Our research aimed to describe histopathologically confirmed NME in dog breeds that hadn't been previously reported. This condition affects a wider spectrum of dog breeds than previously thought.
We wanted to provide preliminary evidence that NME is more common in dog breeds than previously reported.
Materials and Methods
The researchers reviewed archives from 3 institutions and 1 author's collection to identify histopathologically confirmed cases of NME.
They also looked at histology databases from 3 institutions, including Cornell University, Texas A&M University, and the University of California-Davis.
These databases reflected cases referred to Cornell University and were reviewed to identify dogs with NME.
The researchers confirmed the diagnosis of NME by reviewing microscopic slides independently, with 3 pathologists reviewing each case.
Dogs were excluded if central nervous system (CNS) infection was demonstrated or suspected based on histology or further review of available records.
Four dogs that were evaluated by referral centers between 1993 and 2010 were included in the report.
Examination and Results
Necrotizing meningoencephalitis was identified in 4 small dog breeds, including Papillon, Shih Tzu, Coton de Tulear, and Brussels Griffon.
The median age at clinical evaluation was 2.5 years, indicating that this condition typically affects young dogs.
Histopathologic abnormalities included lymphoplasmacytic or histiocytic meningoencephalitis or encephalitis, moderate-to-severe cerebrocortical necrosis, and variable involvement of other anatomic locations within the brain.
Cerebellar herniation through the foramen magnum was confirmed, indicating a significant impact on the brain's structure.
The right parietal lobe was uniformly enlarged with loss of distinction between gray and white matter, and mild hydrocephalus affecting both lateral ventricles was also noted.
Blood vessels in the meninges, gray matter, and white matter were cuffed by a large number of lymphocytes and plasma cells, with fewer macrophage and occasional neutrophils.
No infectious agents or viral inclusions were identified, ruling out other possible causes of the condition.
Microscopically, neuronal necrosis and depletion, marked gliosis, and areas of mild cavitation with gitter cell accumulation were present throughout the cerebrum.
The hippocampus and thalamus had moderate neuronal necrosis and minimal inflammation, while the cerebellum and brainstem were within normal limits.
Dog-Specific Information
Dogs that suffer from necrotizing meningoencephalitis can show a range of symptoms, including seizures, blindness, circling, abnormal mentation, and behavior changes.
Some of the most common symptoms include difficulty walking, back pain, fever, head tilt, falling, facial paralysis, difficulty swallowing, and limb weakness.
The disease typically affects small dog breeds, including Pugs, Maltese, Chihuahuas, Pekingese, Boston terriers, Shih Tzus, Coton du Tulears, and Papillons.
Symptoms can vary depending on the part of the brain affected, with forebrain lesions causing seizures, blindness, and changes in mental status, and brainstem lesions causing head tilt, falling, deafness, and facial paralysis.
Treatment goals focus on providing supportive care and minimizing symptoms, with options including anticonvulsants, corticosteroids, anti-inflammatory medication, chemotherapy, rest, and ensuring proper nutrition and hydration.
Here are some common symptoms of necrotizing meningoencephalitis in dogs:
- Seizures
- Blindness
- Circling
- Abnormal mentation
- Behavior changes
- Difficulty walking
- Back pain
- Fever
- Head tilt
- Falling
- Facial paralysis
- Difficulty swallowing
- Limb weakness
Causes in Dogs
The cause of Necrotizing Meningoencephalitis in dogs is not known, but it's known to develop in certain small dog breeds.
Pugs, Maltese, Chihuahuas, Pekingese, Boston terriers, Shih Tzus, Coton du Tulears, and Papillons are all breeds that can be affected by this disease.
These breeds are often small in size and may be more prone to the disease due to their genetic makeup.
It's essential for dog owners of these breeds to be aware of the symptoms and take preventative measures to reduce the risk of their dog developing this disease.
Some of the breeds that are known to be at risk include the following:
- Pug
- Maltese
- Chihuahua
- Pekingese
- Boston terrier
- Shih Tzu
- Coton du Tulear
- Papillon
Dog 3
Dog 3's story is a heartbreaking one. This Coton de Tulear was presented for multiple episodes of abnormal mentation, generalized tremors, and circling over a 9-month period.
The dog had a 6-week history of progressive obtundation, aggression, and seizures. Its symptoms worsened over time, leading to euthanasia.

A cisternal CSF sample revealed a total nucleated cell count of 108 cells/μL, which is significantly above the normal range of 0-5 cells/μL.
The necropsy results showed asymmetrically distributed areas in both cerebral hemispheres with loss of anatomic distinction in both cortex and underlying white matter.
Microscopically, there was a focal nonsuppurative meningoencephalitis confined to the cerebral hemispheres, with complete sparing of the midbrain and cerebellum.
Here are some possible symptoms of necrotizing meningoencephalitis in dogs, which can vary depending on the affected area of the brain:
- Seizures
- Blindness
- Circling
- Abnormal mentation
- Behavior changes
- Difficulty walking
- Back pain
- Fever
- Head tilt
- Falling
- Facial paralysis
- Difficulty swallowing
- Limb weakness
In the case of Dog 3, the forebrain was likely affected, leading to seizures, blindness, and abnormal mentation.
Recovery in Dogs
The prognosis for dogs with necrotizing meningoencephalitis is poor, but with proper treatment and care, you can help your dog have the best quality of life for as long as possible.
Treatment goals are typically to provide supportive care and minimize your dog's symptoms, as the disease is difficult to treat.
For your interest: Lick Granuloma Dog Home Treatment
Anticonvulsants, such as phenobarbital, are used to treat seizures, while corticosteroids, like dexamethasone or prednisone, are used to suppress your dog's immune system and prevent additional destruction.
Anti-inflammatory medication is also used to help manage your dog's symptoms.
Chemotherapy may be used in some cases, but its effectiveness is not guaranteed.
Rest is crucial for your dog's recovery, as is ensuring he receives proper nutrition and stays well hydrated.
Minimal stress is also essential for your dog's well-being.
Here are some key steps to support your dog's recovery:
- Provide supportive care, such as anticonvulsants and corticosteroids
- Ensure proper nutrition and hydration
- Provide plenty of rest and minimize stress
By following these steps and working closely with your veterinarian, you can help your dog have the best quality of life despite this challenging condition.
Conclusion and Implications
Necrotizing meningoencephalitis is not a breed-restricted disorder, contrary to what was previously thought.
Until now, NME has only been described in 5 small dog breeds, but our cases further illustrate that it's not exclusive to these breeds.
Recent studies have demonstrated that genetic and environmental factors play a role in disease development for other small breed dogs.
NME has been identified worldwide in small, purebred dogs including the Pug, Yorkshire Terrier, Maltese, Chihuahua, and Pekingese.
Histopathologic features of NME include nonsuppurative inflammation of the meninges and brain with extension into the subcortical white matter and deep cortical white matter.
The disease process in NME is multifactorial, with an immune-mediated or autoimmune component to the disease pathogenesis in the Pug and likely other toy breeds.
Risk loci and certain canine leukocyte antigen alleles have been associated with the development of NME, specifically in Pug dogs.
NME is a rapidly progressive, fatal inflammatory brain disorder affecting young dogs.
A fresh viewpoint: Pug Dog Skin Problems
Frequently Asked Questions
Is necrotizing meningoencephalitis contagious?
No, necrotizing meningoencephalitis is not contagious. It's a noninfectious disease, meaning it's not caused by a virus or bacteria that can be spread from one dog to another.
Sources
- https://en.wikipedia.org/wiki/Necrotizing_meningoencephalitis
- https://veterinaryirelandjournal.com/small-animal/352-meningoencephalomyelitis-of-unknown-origin-in-dogs
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895549/
- https://wagwalking.com/condition/necrotizing-meningoencephalitis
- https://avmajournals.avma.org/view/journals/javma/245/11/javma.245.11.1274.xml
Featured Images: pexels.com


